Lyme disease - ME/CFS - Long Covid
Advancements in the Treatment of Complex Chronic Illnesses – A New Center for Patients with Lyme Disease, ME/CFS, and Long COVID
On October 10, 2024, the esteemed Mount Sinai Health System in New York inaugurated the Cohen Center for Recovery From Complex Chronic Illnesses, a state-of-the-art research and treatment facility dedicated to patients suffering from chronic, infection-related diseases. This center focuses on clinical care and scientific exploration of new therapeutic approaches for conditions such as protracted Lyme disease (Lyme+), Long COVID, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and Ehlers-Danlos syndrome (EDS).
While these conditions are increasingly gaining scientific attention, they are by no means new. For years, experts and patients have identified connections between environmental toxins, viral persistence, and immune dysregulation. The Epstein-Barr virus (EBV) has repeatedly been discussed as a potential trigger for ME/CFS and Long COVID, along with the effects of toxic heavy metals and other environmental contaminants. Theories such as those proposed by Anthony William (Medical Medium) — suggesting a link between metal-exposed viruses and neurotoxic processes — raise important questions for further scientific investigation.
Clinical observations suggest that targeted nutritional and environmental
modifications may have a significant impact on the symptoms of patients with ME/CFS, Lyme disease, and Long COVID. These include:
- A gluten-free diet, reduced intake of dairy products, and avoidance of industrial additives
- Minimization of environmental contaminants through air filtration and water purification technologies
- Targeted antiviral strategies for regulating persistent viruses such as EBV
Long-term epidemiological studies are essential to better understand the mechanisms underlying these chronic multisystem illnesses. The central scientific question remains: Is Lyme disease truly a mysterious condition or can environmental factors and viral persistence be identified as primary causes?
Personal Case Study: The Complexity of ME/CFS, Lyme Disease, and Environmental Factors
The diagnosis of chronic illnesses remains a challenging and often prolonged process for many patients. In my personal case, I was repeatedly given a tentative diagnosis of multiple sclerosis (MS), Mastocytosis, mast cell activation syndrome, fibromyalgia, Rheumatoid arthritis or Fabry’s disease. My symptoms — chronic fatigue, itchy skin, tinnitus, severe sleep disturbances, and brain fog — became a constant presence in my daily life. Additionally, I developed arthritis in my knees and ankles, significantly impacting my mobility.
A deeper understanding of the underlying disease mechanisms led to new insights. The globally recognized author Anthony William (Medical Medium) postulates that certain viruses, particularly Epstein-Barr virus (EBV), play a key role in the development of Lyme disease, ME/CFS, and other chronic conditions (2019). He argues that only viruses that feed on toxic heavy metals such as mercury, aluminum and copper — as well as gluten, eggs, dairy products, pesticides, herbicides and fungicides — produce neurotoxins capable of triggering Lyme disease and related multisystem disorders.
Given these insights, my personal healing journey has been guided by a holistic preventive strategy, which includes:
- A strict gluten-free diet for over 14 years, with minimal consumption of eggs and avoid dairy products if possible.
- Targeted reduction of environmental toxins, utilizing air filtration, drinking water purification, nasal filters, and organic produce to minimize exposure to harmful substances.
- Elimination of many preservatives and fragrances, reducing chemical burdens on the body.
- Immune system strengthening and antiviral interventions, aimed at mitigating the effects of persistent EBV infections.
These long-term measures led to significant improvements:
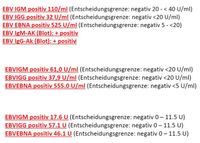
- My IgM Borrelia test remained negative, indicating no further active Lyme disease infections.
- The arthritis in my knees and ankles fully resolved.
- My thymidine kinase levels, a marker for cell proliferation, remained elevated, correlating with ongoing EBV activity.
The central scientific question remains: Is Lyme disease truly a mysterious condition, or can environmental factors and viral persistence be systematically identified as primary causes? As research progresses, we may gain greater clarity on whether environmental toxins, chronic viral infections, and immune dysregulation serve as fundamental drivers of ME/CFS, Lyme disease, and Long COVID.
Dear clinicians, physicians and researchers, please look beyond the horizon and take a look at the website of Medical Medium (Anthony William) and the various successes published there. Kate's case is also my own case and that of many others.
Präsentation eigener Fall / presentation of own case
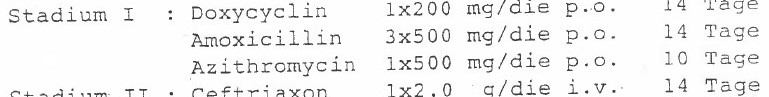
Previously already therapy-resistant Lyme borreliosis with massive ADRs - problem: severe muscle tremors, general restlessness + sinus tachycardi
Antibiotic therapy: immediate discontinuation due to severe intolerance and ADRs
Laboratory Findings and Clinical Course – Analysis of Therapy-Resistant Lyme Disease with Associated Complications
Persistent Lyme Disease and Systemic Effects
The long-term clinical course revealed a therapy-resistant case of Lyme disease, accompanied by severe adverse drug reactions (ADRs). The main complications included:
- Severe muscle tremors, intensifying particularly during resting phases.
- General restlessness, characterized by persistent sleep disturbances and heightened stress responses.
- Sinus tachycardia, indicative of autonomic nervous system dysregulation.
Endocrinological Abnormalities and Suspected Graves’ Disease
During the period when IgM Borrelia tests were positive, fT3 and fT4 levels were significantly elevated, leading to initial suspicion of Graves’ disease.
- In all other phases, particularly after consistent preventive measures, thyroid hormone levels remained within the normal range.
- This suggests a possible inflammation-induced endocrine dysfunction, temporarily causing thyroid hyperactivity.
Sudden Onset of Subacute Arthritis Without Prior Trauma
Another severe manifestation was the sudden onset of subacute arthritis in the right knee and ankle joints, despite the absence of trauma.
- The joint pain and inflammation occurred unexpectedly, pointing to a triggered autoimmune inflammatory response.
- Through targeted preventive strategies, recurrence was successfully prevented, and no further similar symptoms were observed.
Multisystemic Complications Due to Neglected Diagnostic Factors
The worsening condition was primarily driven by a lack of comprehensive diagnostics and insufficient consideration of key factors, including:
- Reactive viruses such as Epstein-Barr Virus (EBV) and Human Herpesvirus 6 (HHV-6)
- Microbiome status and gut flora dysregulation
- Essential micronutrient levels and metabolic imbalances
- Pharmacogenomic (PGx) analysis, which would have been crucial for personalized treatment
Neglecting these essential factors led to progressive health deterioration, with painful and in some cases, life-threatening consequences, particularly due to incorrect medication choices. Only through the implementation of a holistic preventive strategy was a stabilization of my health achieved.
Extended Analysis of the Disease Course – Therapeutic Approaches and Diagnostic Challenges
Ineffective Glucocorticoid Therapy and Progressive Clinical Deterioration
As part of symptomatic treatment, a knee joint puncture with glucocorticoid administration was performed.
- Expected anti-inflammatory effects did not materialize, and instead, the condition worsened.
- Physical weakening significantly increased, suggesting either an ineffective therapeutic approach or a non-inflammatory etiology.
- The final medical assessment concluded unclear genesis, necessitating further diagnostic evaluations.
Diagnosis of Chronic Arthritis and Medication Mismanagement
An orthopedic specialist diagnosed chronic arthritis, which manifested in recurring reactive episodes.
- Initial treatment attempts involved nonsteroidal anti-inflammatory drugs (NSAIDs) and sulfasalazine.
- Both medications led to severe adverse drug reactions (ADRs), requiring immediate discontinuation.
- Years later, pharmacogenomic (PGX) analyses revealed an intolerance to these substances, information that was unavailable at the time.
- Without precise genetic insights, the body continued to weaken, and recovery was significantly hindered.
Laboratory Findings and Suspected Lyme Arthritis – Treatment with Amoxicillin and Clavulanic Acid
- Elevated CRP levels, yet negative rheumatoid factors, making an autoimmune origin less likely.
- Borderline ANA values, providing no definitive rheumatologic diagnosis.
- Lyme arthritis was suspected, leading to antibiotic therapy with clavulanic acid and amoxicillin.
- However, severe ADRs occurred once again, necessitating immediate withdrawal of the medication.
“Seronegative” Lyme Disease and Alternative Explanations
Following repeated serological testing, seronegative Lyme disease was considered.
- An infectious disease expert proposed an alternative hypothesis, suggesting that false-positive serological results might have been caused by B-cell-stimulating viral infections such as EBV, HHV6, CMV, and others.
Lymphocyte Transformation Test – Differentiating Borrelia From Other Viral Factors
A lymphocyte transformation test (LTT) was performed to gain more precise insights into cellular immune responses.
- The test returned a NEGATIVE result for Borrelia, ruling out active Lyme disease.
- However, a significantly elevated basal proliferation rate was detected, most likely driven by EBV-induced immune activation. The stimulation index (SI) revealed the following values:
- Basal proliferation rate: 0.284 OD (Target: < 0.150 OD)
- Interpretation: Systemic T-cell activation, typically seen in acute or chronic infections such as EBV.
Scientific Inquiry
This complex disease course underscores how serological standard diagnostics alone may not always provide a definitive pathogenesis.
- Are Lyme serologies reliable in patients with viral immune dysregulation?
- What role do B-cell-stimulating viruses play in triggering multiple inflammatory reactions?
- How can pharmacogenomic analyses optimize early treatment decisions?
These findings highlight the necessity of multifactorial diagnostics and personalized therapeutic approaches to better understand and effectively treat complex inflammatory conditions such as Lyme disease, ME/CFS, and Long COVID.
Beautiful Dreams of the Future – The Power of Prevention and Perseverance
Even though these vivid impressions still belong to the past for me at the moment and I do not yet have the physical strength for such wonderful sporting activities, I remain committed and disciplined in my preventive journey. Every step forward, every mindful decision has already led to noticeable successes — whether small milestones or significant improvements that strengthen both my body and mind. This progress fills me with pride and renewed hope.
At the same time, we are applying my prevention strategies to help friends and acquaintances struggling with chronic illnesses or Long COVID. And they, too, are achieving remarkable results, reinforcing our determination to continue on this path unwaveringly.
We firmly believe that every effort, every sacrifice, and every challenge will ultimately be worth it. Despite the difficulties, despite the setbacks along the way, we know: Health is a lifelong treasure, one that deserves to be actively protected and nurtured every single day.
And so, we fight each and every day, with radiant smiles on our faces, for our health — paving the way for a future filled with greater vitality, resilience and quality of life.
Long Covid, ME/CFS, EBV & multiple chemical sensitivity (Click here and here)